Introduction
Multiple myeloma is a hematological malignancy characterized by the uncontrolled proliferation of plasma cells within the bone marrow, with an increasing incidence and mortality in the last decade. Eligibility for stem cell transplantation plays a crucial role in determining the approach to treatment, with transplant eligible patients undergoing triple induction therapy with an immunomodulatory agent, a proteasome inhibitor, and steroid. We aimed to review the recent data on the available treatment options for newly diagnosed multiple myeloma (NDMM) in transplant eligible patients.
Methods
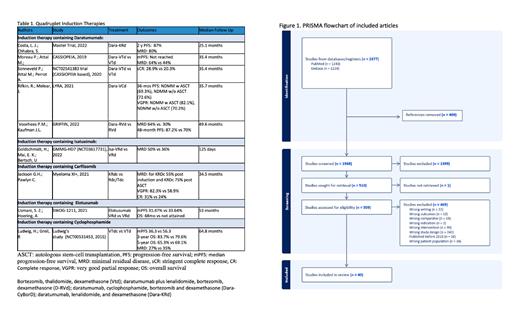
A scoping review was conducted according to the PRISMA 2020 guidelines utilizing the PubMed and Embase databases. The inclusion criteria was phase II or III clinical trials pertaining to the use of triple and quadruple therapy in NDMM patients, from the year 2010 onwards. A total of 2377 search results were screened, with 510 undergoing full-text screening against the inclusion criteria. Covidence was used to facilitate the screening process (Figure 1).
Results
Forty studies were included in the analysis. Eleven trials were based on Daratumumab induction. Additionally, two trials each utilized Isatuximab and Carfilzomib-based induction. One trial employed induction therapy containing Elotuzumab, and another utilized Cyclophosphamide. Addition of Daratumumab to the triplet regimen resulted in significant improvements in response rates and depth of responses. CASSIOPEIA trial demonstrated a notable improvement in minimal residual disease (MRD), with VTd treatment yielding 44% MRD, while Dara-VTd regimens achieved 64% MRD. Similarly, complete response (CR) rates increased from 26% to 39%, respectively. GRIFFIN trial revealed a remarkable 55% reduction in the risk of disease progression for patients with Dara-RVd . Moreover, the estimated 48-month progression-free survival (PFS) rate was 87.2% in the Dara-RVd group, compared to 70% in the RVd group. Notably, the median PFS was not reached in either treatment arm. The Lyra trial, which analyzed Dara-CyBorD followed by Dara maintenance, demonstrated a CR rate of 48.7% for transplant patients and 29.8% for non-transplant patients, respectively. Additionally, the MASTER trial revealed that Dara-KRd/autologous hematopoietic cell transplant (AHCT) led to a high rate of MRD negativity, with 80% of patients achieving MRD negativity. The two-year PFS was 87%. Furthermore, the addition of Isatuximab and Carfilzomib to the treatment regimen demonstrated favorable outcomes in terms of MRD and PFS (Table 1).
The addition of Elotuzumab did not lead to a significant improvement in outcomes. Moreover, caution is warranted when using Cyclophosphamide, given its less favorable safety profile and limited additional benefit in survival outcomes (MRD: 27% in +Cyclophosphamide arm vs. 35% without), including a temporary decline in health-related quality of life.
Conclusion
In conclusion, this scoping review underscores the significance of individualized treatment approaches for multiple myeloma based on clinical trial results. Each induction regimen has shown varying levels of efficacy and safety, offering clinicians flexibility to tailor treatments for different patient populations. The results from these trials will serve as valuable benchmarks and inform future research in the quest for improved therapies for NDMM patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal